How Grains, Sugar, and Seed Oils Drive Fat Storage and Insulin Resistance
Insulin Resistance and Fat Metabolism
Insulin resistance occurs when cells in your muscles, fat, and liver become less responsive to insulin, a hormone critical for regulating blood sugar levels. Diets high in sugar and seed oils can significantly contribute to this condition by "gumming up" insulin receptors, impairing their ability to respond effectively to insulin. Fat cells are less affected by this receptor dysfunction, allowing them to continue storing fat, exacerbating metabolic imbalances.

Grains, especially those high in gluten and antinutrients, can disrupt insulin sensitivity in addition to sugar and seed oils. They contain lectins, which may interfere with nutrient metabolism and exacerbate insulin resistance by binding to cell membranes and disrupting insulin signaling. This can lead to increased intestinal permeability or "leaky gut," promoting inflammation that impairs insulin action even further.
While the fiber in whole grains can help regulate blood sugar by slowing glucose absorption, excessive fiber—particularly without enough fats and proteins—can cause digestive issues. For insulin-resistant individuals, higher fiber intake can worsen gut problems and inflammation, further affecting insulin regulation.
Grains offer more than carbohydrates; they also contain elements such as lectins, phytic acid, and fiber, which also affect insulin sensitivity. If consumed improperly or excessively, these components can contribute to metabolic disorders, including insulin resistance, which can substantially result in weight gain.

How Grains Drive Fat Storage
Grains can contribute to weight gain due to their impact on insulin sensitivity and metabolism:
1. Carbohydrate Content and Insulin Spikes: Grains, especially refined varieties, are high in carbohydrates that convert into glucose. Eating these grains rapidly increases blood sugar levels, prompting the pancreas to release insulin. This hormone helps clear glucose from the blood and store fat. Consistent consumption of high-carbohydrate grains can lead to insulin resistance, a condition in which cells become less responsive to insulin. As a result, the body stores more fat through 'de novo lipogenesis,' which converts excess carbohydrates into fatty acids stored as fat rather than used for energy.
2. Lectins: Found in grains, lectins can bind to insulin receptors and interfere with normal cell signaling. This disrupts glucose uptake and exacerbates insulin resistance, increasing fat storage.
3. Phytic Acid: Phytic acid in grains binds to essential minerals like magnesium and zinc, critical for insulin function. Without these minerals, insulin's efficiency is reduced, contributing to metabolic disorders and weight gain.
4. Fiber and Gut Microbiota: While fiber can be beneficial in moderation, excessive intake of grains, especially insoluble fiber, can negatively alter the gut microbiome. This imbalance can increase inflammation and insulin resistance, promoting weight gain.
By contributing to insulin resistance and disrupting normal metabolic processes, grains create a cycle where the body favors fat storage over fat burning, leading to weight gain over time.
By contributing to insulin resistance and disrupting normal metabolic processes, grains create a cycle where the body favors fat storage over fat burning, leading to weight gain over time.
Seed Oils, Ceramides, and Their Impact
Excessive consumption of seed oils, rich in omega-6 fatty acids, promotes the production of ceramides—lipid molecules that interfere with insulin signaling pathways. Ceramides accumulate in tissues, disrupting cellular metabolism and worsening insulin resistance. This is particularly problematic in the liver, where insulin resistance causes increased glucose production, perpetuating high blood sugar levels.
Ceramides directly affect the endoplasmic reticulum (ER), a structure critical for protein folding and cellular function. They create cellular stress that blocks insulin receptor activity.

The Role of Inflammation
Chronic inflammation, driven by excessive omega-6 fatty acids and sugar, compounds the effects of ceramides. Inflammatory signals disrupt insulin signaling pathways, impair mitochondrial function (our energy-producing factories), and worsen cellular energy imbalances, making it increasingly difficult for cells to metabolize glucose effectively.

Mitochondria and Fat Metabolism
Mitochondria, the cell's powerhouses, play a crucial role in glucose and fat metabolism. Diets high in sugar and seed oils generate toxic byproducts that damage mitochondria, reducing their ability to oxidize fatty acids. This impairs energy production and increases fat storage, particularly in tissues like the liver and abdomen.

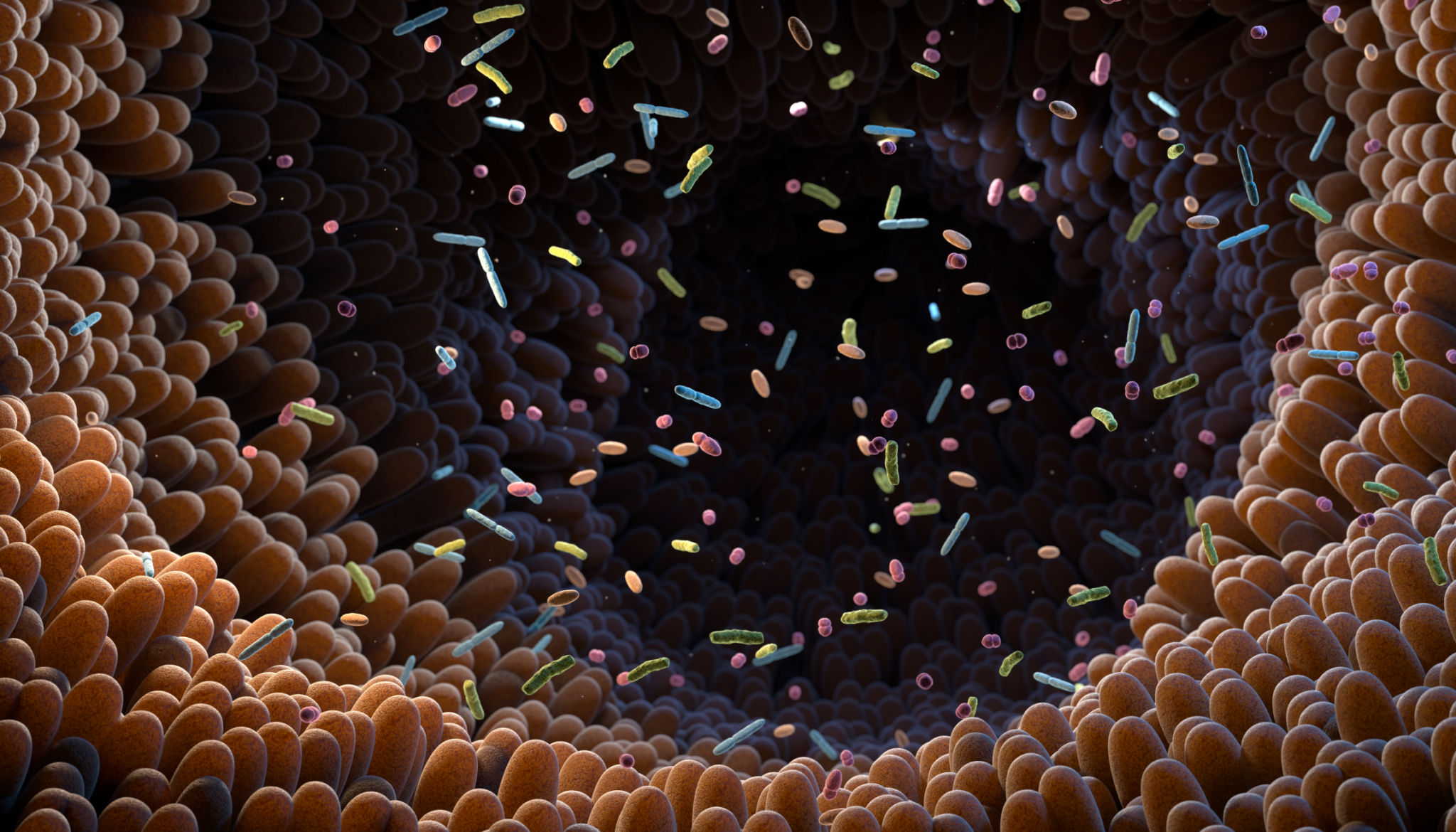
Gut Health and Insulin Resistance
A disrupted gut microbiome, caused by diets high in sugar and seed oils, contributes to systemic inflammation. Harmful bacteria in the gut release lipopolysaccharides (LPS) that enter the liver via the portal vein, worsening liver insulin resistance. A balanced gut microbiome supports nutrient metabolism and helps regulate glucose levels.
Enzymes in Fat Metabolism
Fat metabolism depends on the balance between two key enzymes:
Lipoprotein Lipase (LPL): The Fat Storage Gatekeeper
Lipoprotein lipase (LPL) is an enzyme located on the walls of blood vessels. It acts as a gatekeeper for fat storage by breaking down triglycerides—fat molecules in the bloodstream—into smaller fatty acids. Once broken down, these fatty acids can easily enter fat cells, which are reassembled into triglycerides for long-term storage. LPL activity increases when the body consumes excessive calories, especially carbohydrates and fats, facilitating fat storage.
Hormone-Sensitive Lipase (HSL): Unlocking Stored Fat
Hormone-sensitive lipase (HSL) works inside fat cells to unlock stored energy. When the body requires energy during fasting, exercise, or calorie deficits, HSL breaks down the triglycerides stored in fat cells into free fatty acids and glycerol. These molecules are then released into the bloodstream, where they can be transported to tissues like muscles or the liver to be burned as fuel. HSL activity is suppressed by high insulin levels, which is why diets high in sugar or carbohydrates—leading to elevated insulin—can inhibit fat burning.
Together, these enzymes regulate fat balance: LPL promotes fat storage, while HSL enables fat release for energy. When these enzymes are dysregulated, such as through insulin resistance or chronic overeating, it can lead to weight gain and difficulty losing fat.

The Liver's Central Role in Insulin Resistance
The liver is a metabolic hub that regulates glucose and fat metabolism. In insulin-resistant states, the liver produces glucose despite elevated blood sugar levels. It also converts excess sugar into fat, contributing to fatty liver disease (FLD) and further impairs insulin sensitivity.

Long-Term Consequences
Left unchecked, insulin resistance progresses into type 2 diabetes, cardiovascular diseases, and fatty liver disease. The accumulation of ceramides and chronic inflammation exacerbates cellular dysfunction, perpetuating this cycle of metabolic imbalances.
How to Break the Cycle
- Reduce Seed Oils: Limit processed foods and prioritize healthier fats like those from coconut, avocados, nuts, and olive oil.
- Reduce Excessive Sugar: Reduce high glycemic carbohydrates the strain on insulin receptors.
- Incorporate Anti-inflammatory Foods: Choose whole, antioxidant-rich foods and Omega-3 fatty acids from fatty fish (salmon, mackerel) and fish oil supplements to counter inflammation and ceramide buildup.
- Exercise Regularly: Boost insulin sensitivity and improve glucose uptake into muscles through consistent physical activity.
- Support Gut Health: Opt for soluble fiber-rich and probiotic foods to promote a healthy microbiome.
- Vitamin D: Adequate vitamin D levels are associated with better insulin sensitivity. Sun exposure or supplementation can help.
- Intermittent Fasting: Time-restricted eating or intermittent fasting can reduce fasting insulin levels and improve insulin sensitivity by allowing the body to reset its metabolic processes.

Conclusion
Understanding the biochemical effects of seed oils and sugar on insulin resistance reveals how modern dietary habits drive metabolic dysfunction. From "gumming up" insulin receptors to promoting ceramide buildup, these substances impair cellular processes, inflame tissues, and disrupt fat metabolism. The liver, enzymes like LPL and HSL, and mitochondrial health all play pivotal roles in this complex web. Adopting a diet rich in whole foods, healthy fats, antioxidants, and regular exercise can restore insulin sensitivity and support overall metabolic health. Small, consistent changes pave the way to lasting wellness.
